Infectious Disease Exposure Risks a Top Workplace Concern in 2026
January 13, 2026 | General
The persistent risk of exposure to infectious diseases – an invisible threat – is a top concern for U.S. employers. WorkCare provides solutions to help employers prevent sickness absence, reduce medical costs, and avoid disruptions in operations.
This is the second part of a series of articles on WorkCare solutions that align with critical occupational health and safety exposure risks and other top-of-mind concerns as U.S. employers begin the new year and develop long-term intervention strategies.
Infectious Diseases in the Workplace
The lingering effects of the COVID-19 pandemic remain a top concern for U.S. employers in 2026. The pandemic raised extraordinary workplace environment, health, and safety challenges. The rapid spread of coronavirus disease heightened awareness of infectious disease exposure risks and upended the way Americans do their jobs.
At the start of 2026, U.S. public health officials were monitoring a sharp uptick in influenza (flu) cases, which is associated with three to six days of work absence for normally healthy employees. Other infectious agents that are constantly monitored include COVID-19 variants, measles, RSV, pertussis (whooping cough), malaria, and tick-borne illnesses, along with a lengthy list of emerging infectious diseases like Mpox, Marburg, Ebola, and Dengue. Previously unidentified pathogens are detected when they appear in a limited population, spread to other geographic regions, or symptoms do not respond to standard treatments, according to the Infectious Disease Society of America.
People are exposed to germs every day and do not get sick because they develop resistance to them over time. They are more vulnerable when they do not take standard precautions, like frequent hand-washing, have a weak immune system or underlying disease, don’t get enough sleep, are under stress, or generally feel rundown. Infants and frail elderly people are particularly susceptible to serious illness.
Why Employers Should Pay Attention to Infectious Diseases
Infectious diseases can cause acute sickness, chronic illness, and death, with significant related costs for employers and society:
- Vaccine-preventable infectious diseases cost the U.S. economy an estimated $8.9 billion in 2024, according to the National Foundation for Infectious Diseases.
- The flu alone is annually associated with billions of dollars in lost productivity, plus the cost of outpatient and inpatient care, the National Committee on Quality Assurance and National Alliance on Healthcare Purchaser Coalition reported during the COVID-19 pandemic.
- A University of South Florida study published in the Journal of Occupational and Organization Psychology found that workplace cultures in which employees feel pressured to work when they are sick have measurable declines in overall workforce productivity and retention rates.
How High is the Infectious Disease Exposure Risk?
A systematic review of infectious disease exposure risk published in Occupational & Environmental Medicine found that workers in healthcare and laboratory settings, and in jobs that involve contact with animals or refuse, have the highest risk of exposure to infectious pathogens. First responders, agriculture workers and those in occupations that involve food service, transportation, or contact with children also have higher-than-average risk of exposure to contagious diseases.
Contagious disease outbreaks in the workplace typically occur when employees have unprotected contact with sick co-workers and household members, infected blood or feces, or contaminated surfaces. Some illnesses are spread via invisible airborne droplets that are inhaled. Microbes can enter the body through membranes or breaks in the skin. In some cases, an infected animal or insect passes a disease to a human host, or a person ingests contaminated food or water.
Which OSHA Standards Apply?
OSHA enforces standards to protect employees with infectious disease exposure risk. Failure to comply can result in citations, fines, and loss of business. Applicable standards include the General Duty Clause, which requires employer to provide a workplace free from recognized hazards that cause or are likely to cause death or serious physician harm. These standards apply to specific conditions:
· Bloodborne Pathogens, 1910.1030 – Applies to all routes of exposure to blood and other potentially infectious materials defined in the standard, including soiled laundry, sharps, and devices used to administer medication or fluids. Pathogens of concern include HIV (the virus that causes AIDS), and hepatitis B and C. Incidents involving unprotected exposure requires an immediate response, including post-exposure procedures to ensure compliance, protect employee health and safety, and reduce legal liability.
· Personal Protective Equipment, 1910.132 – Applies to the use of PPE to protect the eyes, face, head, and extremities. PPE may include protective clothing, shields and barriers, and respiratory devices. An estimated 40% of occupational diseases and injuries could be prevented with proper use of PPE.
· Respiratory Protection, 1910.134 – Applies to occupations with risk of exposure to infectious agents and other respiratory hazards. Respirators must be worn when effective engineering controls are not feasible to use. Respirator medical evaluation and fit-test procedures are used to ensure proper selection of a respirator designed for the job and a correct fit.
What Can Employers Do for Infectious Disease Prevention?
Employers are advised to:
1. Monitor and mitigate conditions that can contribute to the spread of germs in the workplace. Examples include:
- High population density requiring close proximity while working
- Sharing equipment, workstations, locker rooms, and breakrooms
- Heating, cooling, and ventilation systems that are not well maintained
- Unenforced personal hygiene and workplace cleanliness policies
- Employees who work when they are sick due to fear of job and monetary loss
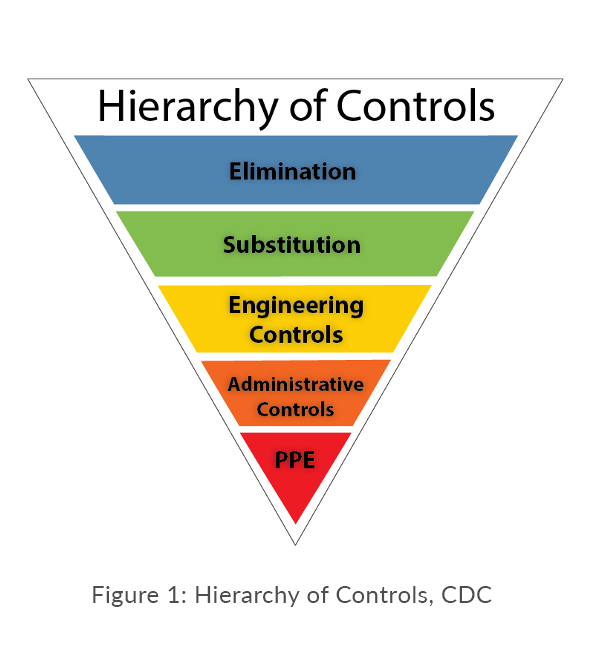
2. Use the hierarchy of controls as the foundation for infectious disease prevention in the workplace. The CDC recommends focusing first on elimination, substitution, and engineering controls because they do not depend on human interaction. Training is essential when using administrative controls and PPE because consistency is necessary to reduce exposure risk. (See Figure 1.) The CDC’s core infection prevention and control practices for the safe delivery of healthcare services applies to all healthcare settings.
3. Monitor employee compliance with controls like hand-washing, use of PPE (gloves, masks, gowns, eye protection, respiratory protection), isolation, adequate ventilation, and barriers, as needed.
4. Provide free or low-cost vaccinations to employees who wish to receive them. Vaccination is considered to be the first line of defense against the flu, chickenpox, shingles, and certain other infectious agents. (Refer to our fact sheet on Fighting the Flu with a Workplace Prevention Campaign.)
5. Use multiple communication platforms and methods to inform workers about contagious disease risks, ways to protect vulnerable populations, how to help prevent the spread of illness in workplaces, at home, and in communities, and recommended remedies for symptoms.
How WorkCare Helps
At WorkCare, we help employers prepare for and monitor seasonal outbreaks of contagious illnesses and the emergence of new pathogens that require flexible, adaptable workplace policies. For example, during the COVID-19 pandemic we had all hands on deck providing up-to-date clinical information and operational recommendations. We successfully implemented site-specific protective measures, and our occupational health providers offered the reassurance that employees needed to safely do their jobs.
Our business is dedicated to protecting and promoting employee health – from hire to retire. This includes the delivery of in-person and remote-access education on contagious disease threats, vaccinations, travel advisories, symptom recognition, and care guidance. WorkCare business divisions on the front lines of disease prevention include:
- Occupational Health Screening, including fitness-for-work evaluations after a sickness absence.
- Incident Prevention, offering wellness educators and prevention specialists who collaborate with employers to keep their employees healthy, safe, and productive.
- On-Site Clinical Services, with occupational health providers on duty to provide preventive interventions, symptom evaluation, and immediate care.
- Exposure Risk Assessment and Medical Monitoring, offering expert management of medical surveillance programs for biological and other potentially infectious hazards in labs, manufacturing facilities, and healthcare organizations.
- Immunizations and Medications, including flu shots and business travel-related immunizations in all types of industries that are provided on-site or by referral to qualified local providers.
“We have a long history of helping employers comply with medical surveillance requirements by engaging with their employees, answering their health-related questions, and providing resources to help prevent the spread of preventable infectious diseases that interfere with livelihoods and business operations.”
– Peter P. Greaney, M.D., Founder, Executive Chairman, and Chief Medical Officer, WorkCare
FAQs
Q: What is the likelihood of another pandemic occurring within the next 10 years?
A: Experts say a pandemic is relatively likely to occur within the next decade. For example, Airfinity, Ltd., a company specializing in predictive health intelligence and data analytics, used a model to project a 27.5% chance for a deadly pandemic, which aligns with other organizations’ projections, including the insurance industry. Airfinity also predicts that rolling out effective vaccines within 100 days of discovering a new pathogen would reduce the likelihood of a pandemic to 8.1%. Factors influencing global spread of disease include climate change, population expansion, growth in international travel, and emerging zoonotic diseases(germs carried by animals).
Q: Are vaccinations 100 percent effective at preventing illness?
A: No, vaccination is not 100% effective, but it is a safe way to help prevent sickness, reduce symptom severity, stop the spread of disease, and save lives. The more people who are vaccinated, the greater the protection afforded to everyone. This is called herd or group immunity. Refer to the Institute for Vaccine Safety at Johns Hopkins University, the World Health Organization, and the CDC for related resources.
Q: In addition to vaccination, what are some simple ways to reduce contagious illness exposure risk?
A: Easy prevention measures include:
- Frequently washing hands with warm water and soap for 20 seconds or using hand sanitizer.
- Wearing a mask when in crowds and near vulnerable people, like the elderly, infants, and those with compromised immune systems.
- Covering coughs and sneezes and disposing used tissues in a covered receptacle.
- Staying home when feeling ill or after a known exposure to a contagious illness.
- Washing surfaces and utensils after handling raw meat, seafood, or eggs, rinsing fresh produce in clean water, following cooking directions (time and temperature), and storing perishable foods in the refrigerator.
Stay connected and get the latest updates from WorkCare
Let’s Work Together
Ready to take your workforce health and safety to the next level?
Contact us today to learn how WorkCare can partner with you to create a healthier, safer, and more productive workplace.